When writer, speaker, and former television news anchor Dina Ruiz talked to a journalism class at California State University, Monterey Bay, she impressed upon her young audience the message that knowledge truly is power. And she has a potentially lifesaving story to illustrate her point.
Luba also co-directs Montage Health’s Genetic Risk Assessment program with Dr. Lulu Zhang, a hematology and medical oncology specialist. Launched in 2022 with grant support from Montage Health Foundation for a pilot, the program empowers Monterey County residents — like Dina — and their relatives to make informed decisions about screenings and treatments for inherited cancers through risk assessment and genetic testing.
“One out of every 25 to 50 people has a genetic mutation that increases cancer risk,” Luba says. “People can take steps to help prevent that cancer from developing or catch the cancer at a curable stage.”
Dina, then 57, has a history of gastric (stomach) cancer on both sides of her family and had recently lost her mother to the disease. She decided to get screened.
She went to Montage Health’s Carol Hatton Breast Care Center, where every patient who gets a mammogram can receive a risk assessment and subsequent genetic testing through the Genetic Risk Assessment program if screening results indicate an increased risk.
Dina’s initial screening indicated an increased cancer risk, as expected due to her family history of gastric cancer. But she was surprised to learn that she had the BRCA2 gene, a mutation that dramatically increases risk for breast and ovarian cancers.
One out of every 25 to 50 people has a genetic mutation that increases cancer risk. People can take steps to help prevent that cancer from developing or catch the cancer at a curable stage.
— Dr. Daniel Luba, gastroenterologist and internal medicine specialist
“A few weeks after I took the genetic test,” Dina says, “I was notified that I tested positive for the BRCA2 mutation. I went to my car and cried for 5 minutes. Then, with this knowledge, I felt extremely empowered to be able to get a hold on this before I developed cancer. What a gift.”
Dina called her daughter, Morgan Eastwood, then 25, to let her know. Because of her own results, her daughter had a 50 percent chance of also having the mutation. Morgan took the test, and the results were the same: She also carries the BRCA2 mutation.
“The results were shocking,” Morgan says. “But we have empowered ourselves with this information. My mom and I are great about keeping up with our health and visiting our doctors, so we looked at the information as a blessing, something we can get in front of and take care of before anything bad manifests.”
Two months after Dina learned she has the BRCA2 mutation, she underwent preventive surgery and had her ovaries removed.
“They found a cyst on my right ovary the size of an egg but no cancer cells,” she says. “How lucky am I?”
In the meantime, while Morgan has decisions to make about the preventive measures she will take, she is first experiencing the rites of passage the same preventive surgery would eliminate. She and her husband welcomed their first child in September and hope to have at least one more before she has her ovaries removed.
“I have to start thinking about some major decisions,” says Morgan, now 27, “including a possible mastectomy. It’s a lot to think about but I’m grateful to be aware so I can make proactive decisions about my health.”
Take this short survey to identify your cancer risk factors and get a recommended prevention plan.
Cancer screening recommendations
Screening tests check for signs of a health problem before you experience symptoms. Regular screenings can help you detect cancer early, when it’s most treatable. The screenings you need depend on your age, gender, family health history, and other factors.
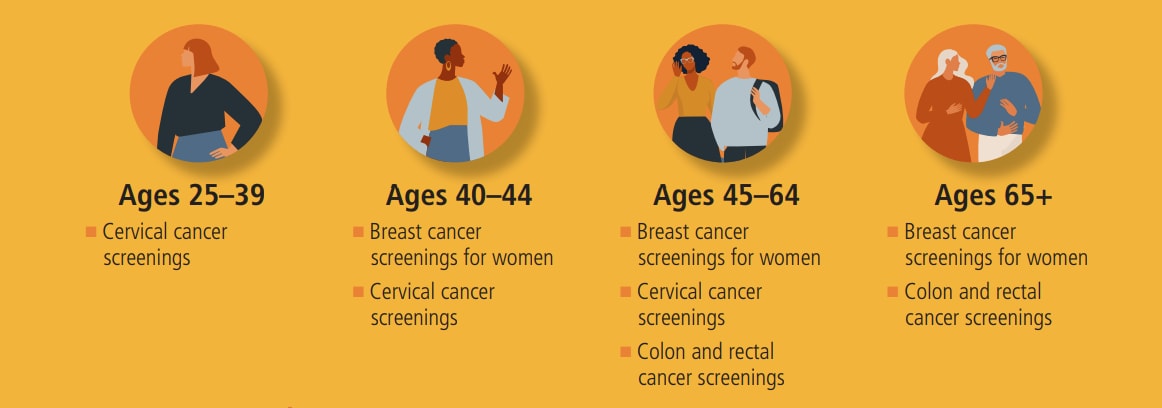
Breast cancer screenings
Women should get mammograms every one to two years starting at age 40, or as instructed by their doctor.
Cervical cancer screenings
The American Cancer Society’s general screening guidelines say that women between ages 25 and 65 should have a Pap test every three years or a combined Pap and HPV test every five years. For those older than 65:
- If you’ve had regular cervical cancer testing with normal results, you no longer need to be screened
- If you have a history of cervical precancer, continue to get tested for at least 20 years after that diagnosis
Colon and rectal cancer screenings
At age 45, men and women at average risk should begin colorectal cancer screenings. Options include:
- Colonoscopy performed every 10 years or as instructed by a doctor
- CT colonography performed every five years or as instructed by a doctor
- Fecal immunochemical test (FIT) performed yearly or as instructed by a doctor
- FIT-DNA test performed every three years or as instructed by a doctor
- Sigmoidoscopy performed every five years or as instructed by a doctor